Abstract
Purpose
To estimate associations between multiple forms of substance use with self-harming thoughts and behaviours, and to test whether gender is an effect modifier of these associations, both independently and along with perceived risk of cannabis use.
Methods
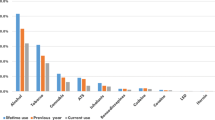
Data were drawn from the 2018 Norwegian Students’ Health and Wellbeing Study (SHoT 2018). A national sample of n = 50,054 full-time Norwegian students (18–35 years) pursuing higher education completed a cross-sectional student health survey, including questions on past-year self-harm: non-suicidal thoughts of self-harm, non-suicidal self-harm, suicidal thoughts, and suicide attempt. Students reported their frequency of past-year alcohol use (range: never to ≥ 4 times/ week), illicit substance consumption, and perceived risk of cannabis use. The AUDIT and CAST screening tools measured problematic alcohol and cannabis consumption, respectively. We used logistic regression modelling adjusted for age, symptoms of depression and anxiety, and financial hardship (analytic sample range: n = 48,263 to n = 48,866).
Results
The most frequent alcohol consumption category (≥ 4 times/ week) was nearly always associated with more than a two-fold increased likelihood of self-harm. Less frequent alcohol consumption was associated with reduced odds of suicidal thoughts [monthly or less: OR = 0.87 (95% CI: 0.75–1.00), 2–4 times/month: OR = 0.79 (95% CI: 0.69–0.91), and 2–3 times/ week: OR = 0.83 (95% CI: 0.71–0.98)]. Problematic alcohol consumption was associated with most outcomes: odds ranging from 1.09 (95% CI: 1.01–1.18) for suicidal thoughts to 1.33 (95% CI: 1.00–1.77) for suicide attempt. There was evidence of multiple illicit substance by gender interactions: consumption of all but one illicit substance category (other drug use) was associated with all four forms of self-harm for women, but findings among men were less clear. Among men, only one illicit substance category (stimulant) was associated with most forms of self-harm. Women, but not men, who perceived cannabis use as a health risk were more likely to experience non-suicidal thoughts as cannabis consumption increased, and with harmful consumption patterns.
Conclusion
Frequent alcohol consumption is associated with increased risk of self-harm and suicidality for young women and men. Associations between illicit substance use and self-harm and suicidality appear stronger in women compared to men.
Similar content being viewed by others
Data availability
Details regarding data access are available from the Norwegian Institute of Public Health (https://www.fhi.no/en/more/access-to-data/).
Code availability
STATA code can be made available upon request.
References
Heradstveit O, Skogen JC, Brunborg GS, Lønning KJ, Sivertsen B (2019) Alcohol-related problems among college and university students in Norway: extent of the problem. Scand J Public Health. https://doi.org/10.1177/1403494819863515
Heradstveit O, Skogen JC, Edland-Gryt M et al (2020) Self-reported illicit drug use among Norwegian university and college students Associations with age, gender, and geography. Front Psychiatry 11:543507. https://doi.org/10.3389/fpsyt.2020.543507
Arria AM, Caldeira KM, O’Grady KE et al (2008) Drug exposure opportunities and use patterns among college students: results of a longitudinal prospective cohort study. Subst Abus 29:19–38. https://doi.org/10.1080/08897070802418451
Nordfjærn T, Bretteville-Jensen AL, Edland-Gryt M, Gripenberg J (2016) Risky substance use among young adults in the nightlife arena: an underused setting for risk-reducing interventions? Scand J Public Health 44:638–645. https://doi.org/10.1177/1403494816665775
Davoren MP, Demant J, Shiely F, Perry IJ (2016) Alcohol consumption among university students in Ireland and the United Kingdom from 2002 to 2014: a systematic review. BMC Public Health 16:173. https://doi.org/10.1186/s12889-016-2843-1
United Nations (2020) World drug report 2020: booklet 2, drug use and health consequences (No. E.20.XI.6). United Nations publication. https://wdr.unodc.org/wdr2020/en/drug-use-health.html. (Accessed 18 Janu 2021)
Gobbi G, Atkin T, Zytynski T et al (2019) Association of cannabis use in adolescence and risk of depression, anxiety, and suicidality in young adulthood: a systematic review and meta-analysis. JAMA Psychiat 76:426. https://doi.org/10.1001/jamapsychiatry.2018.4500
Carliner H, Brown QL, Sarvet AL, Hasin DS (2017) Cannabis use, attitudes, and legal status in the U.S.: a review. Prevent Med 104:13–23. https://doi.org/10.1016/j.ypmed.2017.07.008
Burdzovic Andreas J, Sivertsen B, Lønning KJ, Skogen JC (2021) Cannabis use among Norwegian university students: gender differences, legalization support and use intentions, risk perceptions, and use disorder. Addict Behav Rep 13:100339. https://doi.org/10.1016/j.abrep
Richardson E, DePue MK, Therriault DJ, Alli S, Liu R (2020) The influence of substance use on engagement in non-suicidal self-injury (NSI) in adults. Subst Use Misuse 55:89–94. https://doi.org/10.1080/10826084.2019.1656254
Sivertsen B, Hysing M, Knapstad M et al (2019) Suicide attempts and non-suicidal self-harm among university students: prevalence study. BJPsych Open 5:e26. https://doi.org/10.1192/bjo.2019.4
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders fifth edition. American Psychiatric Association, Arlington
Klonsky ED, May AM, Glenn CR (2013) The relationship between nonsuicidal self-injury and attempted suicide: converging evidence from four samples. J Abnorm Psychol 122:231–237. https://doi.org/10.1037/a0030278
Mars B, Heron J, Klonsky ED et al (2019) Predictors of future suicide attempt among adolescents with suicidal thoughts or non-suicidal self-harm: a population-based birth cohort study. Lancet Psychiatry 6:327–337. https://doi.org/10.1016/S2215-0366(19)30030-6
Selby EA, Kranzler A, Fehling KB, Panza E (2015) Nonsuicidal self-injury disorder: the path to diagnostic validity and final obstacles. Clin Psychol Rev 38:79–91. https://doi.org/10.1016/jcpr.2015.03.003
Miranda-Mendizabal A, Castellví P, Parés-Badell O et al (2019) Gender differences in suicidal behavior in adolescents and young adults: systematic review and meta-analysis of longitudinal studies. Int J Public Health 64:265–283. https://doi.org/10.1007/s00038-018-1196-1
Cipriano A, Cella S, Cotrufo P (2017) Nonsuicidal self-injury: a systematic review. Front Psychol 8:1946. https://doi.org/10.3389/fpsyg.2017.01946
Victor SE, Muehlenkamp JJ, Hayes NA, Lengel GJ, Styer DM, Washburn JJ (2018) Characterizing gender differences in nonsuicidal self-injury: evidence from a large clinical sample of adolescents and adults. Compr Psychiatry 82:53–60. https://doi.org/10.1016/jcomppsych.2018.01.009
Griffin K, Twynstra J, Gilliland JA, Seabrook JA (2021) Correlates of self-harm in university students: a cross-sectional study. J Am Coll Health. https://doi.org/10.1080/07448481.2021
Valen A, Bogstrand ST, Vindenes V, Gjerde H (2017) Increasing use of cannabis among arrested drivers in Norway. Traffic Inj Prev 18:801–806. https://doi.org/10.1080/15389588.2017
Sivertsen B, Råkil H, Munkvik E, Lønning KJ (2019) Cohort profile: the SHoT-study, a national health and well-being survey of Norwegian university students. BMJ Open 9:e025200. https://doi.org/10.1136/bmjopen-2018-025200
OECD (2009) OECD Reviews of Tertiary Education: Norway 2009. OECD publication. https://www.oecd-ilibrary.org/education/oecd-reviews-of-tertiary-education-norway-2009_9789264039308-en. (Accessed 12 Sept 2021)
OECD (2021) Population with tertiary education (indicator). OECD data. https://doi.org/10.1787/0b8f90e9-en. (Accessed 12 September 2021)
European Monitoring Centre for Drugs and Drug Addiction (2015) ESPAD 2015 methodology. The European School Survey Project on Alcohol and Other Drugs. http://www.espad.org/reports-documents. (Accessed 18 Janu 2021)
Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M (1993) Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption–II. Addiction 88:791–804. https://doi.org/10.1111/j.1360-0443.1993.tb02093.x
Jensen P, Haug E, Sivertsen B, Skogen JC (2021) Satisfaction with life, mental health problems and potential alcohol-related problems among Norwegian university students. Front Psychiatry 12:578180. https://doi.org/10.3389/fpsyt.2021.578180
Legleye S, Karila L, Beck F, Reynaud M (2007) Validation of the CAST, a general population Cannabis Abuse Screening Test. J Subst Use 12:233–242. https://doi.org/10.1080/14659890701476532
Legleye S (2018) The Cannabis Abuse Screening Test and the DSM-5 in the general population: optimal thresholds and underlying common structure using multiple factor analysis. Int J Methods Psychiatr Res 27:e1597. https://doi.org/10.1002/mpr.1597
Madge N, Hewitt A, Hawton K et al (2008) Deliberate self-harm within an international community sample of young people: comparative findings from the Child & Adolescent Self-harm in Europe (CASE) Study. J Child Psychol Psychiatry 49:667–677. https://doi.org/10.1111/j.1469-7610.2008.01879.x
McManus S, Bebbington P, Jenkins R, Brugha T, eds (2016) Mental health and wellbeing in England: adult psychiatric morbidity survey 2014. NHS Digital. https://digital.nhs.uk/data-and-information/publications/statistical/adult-psychiatric-morbidity-survey/adult-psychiatric-morbidity-survey-survey-of-mental-health-and-wellbeing-england-2014. (Accessed 18 Janu 2021)
Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L (1974) The Hopkins Symptom Checklist (HSCL): a self-report symptom inventory. Behav Sci 19:1–15. https://doi.org/10.1002/bs.3830190102
Skogen JC, Øverland S, Smith ORF, Aarø LE (2017) The factor structure of the Hopkins symptoms checklist (HSCL-25) in a student population: a cautionary tale. Scand J Public Health 45:357–365. https://doi.org/10.1177/1403494817700287
Pacek LR, Mauro PM, Martins SS (2015) Perceived risk of regular cannabis use in the United States from 2002 to 2012: differences by sex, age, and race/ethnicity. Drug Alcohol Depend 149:232–244. https://doi.org/10.1016/j.drugalcdep.2015.02.009
Bøe T, Hysing M, Siversten B (2019) Higher education students’ mental health problems: results from the Norwegian SHOT study. Eur J Public Health 29(ckz185):023. https://doi.org/10.1093/eurpub/ckz185.023
Ribeiro JD, Huang X, Fox KR, Franklin JC (2018) Depression and hopelessness as risk factors for suicide ideation, attempts and death: meta-analysis of longitudinal studies. Br J Psychiatry 212:279–286. https://doi.org/10.1192/bjp.2018.27
Bentley KH, Franklin JC, Ribeiro JD, Kleiman EM, Fox KR, Nock MK (2016) Anxiety and its disorders as risk factors for suicidal thoughts and behaviors: a meta-analytic review. Clin Psychol Rev 43:30–46. https://doi.org/10.1016/j.cpr.2015.11.008
MacKinnon N, Colman I (2016) Factors associated with suicidal thought and help-seeking behaviour in transition-aged youth versus adults. Can J Psychiatry 61:789–796. https://doi.org/10.1177/070674371666741
Villarosa MC, Messer MA, Madson MB, Zeigler-Hill V (2018) Depressive symptoms and drinking outcomes: the mediating role of drinking motives and protective behavioral strategies among college students. Subst Use Misuse 53:143–153. https://doi.org/10.1080/10826084.20171327974
Bilevicius E, Single A, Rapinda KK, Bristow LA, Keough MT (2018) Frequent solitary drinking mediates the associations between negative affect and harmful drinking in emerging adults. Addict Behav 87:115–121. https://doi.org/10.1016/j.addbeh.2018.06.026
Evans-Polce RJ, Schuler MS, Schulenberg JE, Patrick ME (2018) Gender- and age-varying associations of sensation seeking and substance use across young adulthood. Addict Behav 84:271–277. https://doi.org/10.1016/j.addbeh.2018.05.003
Lockwood J, Townsend E, Daley D, Sayal K (2020) Impulsivity as a predictor of self-harm onset and maintenance in young adolescents: a longitudinal prospective study. J Affect Disord 274:583–592. https://doi.org/10.1016/j.jad.2020.05.021
Centre for Addiction and Mental Health (CAMH) (2014) Cannabis policy framework. CAMH. http://www.camh.ca/-/media/files/pdfs---public-policy-submissions/camhcannabispolicyframework-pdf.pdf. (Accessed 18 Janu 2021)
Mortier P, Auerbach RP, Alonso J et al (2018) Suicidal thoughts and behaviors among college students and same-aged peers: results from the World Health Organization World Mental Health Surveys. Soc Psychiatry Psychiatr Epidemiol 53:279–288. https://doi.org/10.1007/s00127-018-1481-6
Maggs JL, Staff J, Kloska DD, Patrick ME, O’Malley PM, Schulenberg J (2015) Predicting young adult degree attainment by late adolescent marijuana use. J Adolesc Health 57:205–211. https://doi.org/10.1016/j.jadohealth.2015.04.028
Moller CI, Tait RJ, Byrne DG (2013) Deliberate self-harm, substance use, and negative affect in nonclinical samples: a systematic review. Subst Abus 34:188–207. https://doi.org/10.1080/08897077.2012.693462
Regehr C, Glancy D, Pitts A (2013) Interventions to reduce stress in university students: a review and meta-analysis. J Affect Disord 148:1–11. https://doi.org/10.1016/j.jad.2012.11.026
Kessler RC (2000) Psychiatric epidemiology: selected recent advances and future directions. Bull World Health Organ 78(464–474):11
Chalmers J, Lancaster K, Hughes C (2016) The stigmatisation of ‘ice’ and under-reporting of meth/amphetamine use in general population surveys: a case study from Australia. Int J Drug Policy 36:15–24
Anderssen N, Sivertsen B, Lønning KJ, Malterud K (2020) Life satisfaction and mental health among transgender students in Norway. BMC Public Health 20:138. https://doi.org/10.1186/s12889-020-8228-5
Moran P, Coffey C, Romaniuk H, Degenhardt L, Borschmann R, Patton GC (2015) Substance use in adulthood following adolescent self-harm: a population-based cohort study. Acta Psychiatr Scand 131:61–68. https://doi.org/10.1111/acps.12306
Chung WW, Hudziak JJ (2017) The transitional age brain: “the best of times and the worst of times.” Child Adolesc Psychiatr Clin N Am 26:157–175. https://doi.org/10.1016/j.chc.2016.12017
Duffy A, Saunders KEA, Malhi GS et al (2019) Mental health care for university students: a way forward? Lancet Psychiatry 6:885–887. https://doi.org/10.1016/S2215-0366(19)30275-5
Gardner W, Pajer K, Cloutier P et al (2019) Changing rates of self-harm and mental disorders by sex in youths presenting to Ontario emergency departments: repeated cross-sectional study. Can J Psychiatry 64:789–797. https://doi.org/10.1177/0706743719854070
Acknowledgements
We wish to thank all students participating in the study, as well as the three largest student welfare organizations in Norway (SiO, Sammen, and SiT), who initiated and designed the SHoT study.
Funding
This work was partly supported by the Research Council of Norway through its Centres of Excellence funding scheme (project number 262700), the Canada Research Chairs program, and by the Frederick Banting and Charles Best Canada Graduate Scholarship Doctoral Awards (CGS-D) program. SHoT2018 has received funding from the Norwegian Ministry of Education and Research (2017) and the Norwegian Ministry of Health and Care Services (2016).
Author information
Authors and Affiliations
Contributions
All authors contributed to study conceptualization and design. Data analysis was performed by Dr. IC. The first draft of the manuscript was prepared by Ms. NGH. All authors provided feedback and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Role of the funder
The Research Council of Norway, the Canada Research Chairs program, and the CGS-D program had no role in study design, data collection or analysis, nor did they influence the authors’ decision to prepare and publish this manuscript.
Ethics approval
The Regional Committee for Medical and Health Research Ethics in Western Norway approved SHoT2018 (no. 2017/1176).
Consent to participate
Participants provided informed consent (electronically).
Consent for publication
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary materials.
Rights and permissions
About this article
Cite this article
Hammond, N.G., Sivertsen, B., Skogen, J.C. et al. The gendered relationship between illicit substance use and self-harm in university students. Soc Psychiatry Psychiatr Epidemiol 57, 709–720 (2022). https://doi.org/10.1007/s00127-021-02209-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-021-02209-3